What is an IV Set for Dialysis?
An IV Set for Dialysis refers to the intravenous tubing and related accessories used during hemodialysis or peritoneal dialysis treatments. The IV set ensures proper fluid management and medication administration during dialysis, providing crucial support to the dialysis process.
Purpose of IV Set in Dialysis
IV sets are essential for delivering fluids, anticoagulants, and medications throughout the dialysis process. They help maintain the patient’s fluid balance and prevent complications such as clotting in the dialysis circuit.
Key Components of an IV Set for Dialysis
-
IV Tubing – Flexible, sterile tubing designed for fluid transport.
-
Drip Chamber – Visualizes the flow of fluids and eliminates air bubbles.
-
Injection Ports – Allow the administration of medications or heparin.
-
Roller Clamp – Controls the rate at which fluids are infused.
-
Luer Lock Connector – Securely connects the IV set to the catheter or dialysis circuit.
-
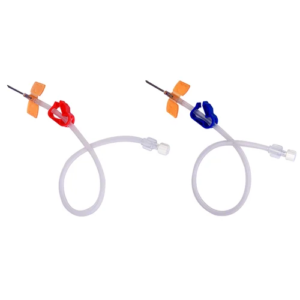
Needles/Catheters (if standalone) – Used for direct vascular access, often paired with fistula needles or dialysis catheters.
Common Uses in Dialysis
-
Heparin administration to prevent blood clotting in the dialysis circuit.
-
Saline flushes to maintain patency of the dialysis access.
-
Medications (such as erythropoietin, antibiotics) given during dialysis.
-
Volume resuscitation in emergencies when fluid needs to be administered.
Important Notes
-
IV sets for dialysis must be sterile and pyrogen-free to reduce infection risks.
-
Typically designed as single-use to ensure safety.
-
Some IV sets are pre-connected to heparin lines or include Y-sites for flexibility.
Summary
An IV Set for Dialysis is a vital component of dialysis treatment, ensuring safe fluid delivery, medication administration, and anticoagulation during the procedure. It includes key components like IV tubing, drip chambers, and injection ports, and is primarily used for heparin infusion, saline flushes, and medication delivery. Always ensure the IV set is sterile and single-use to minimize infection risks and ensure patient safety.